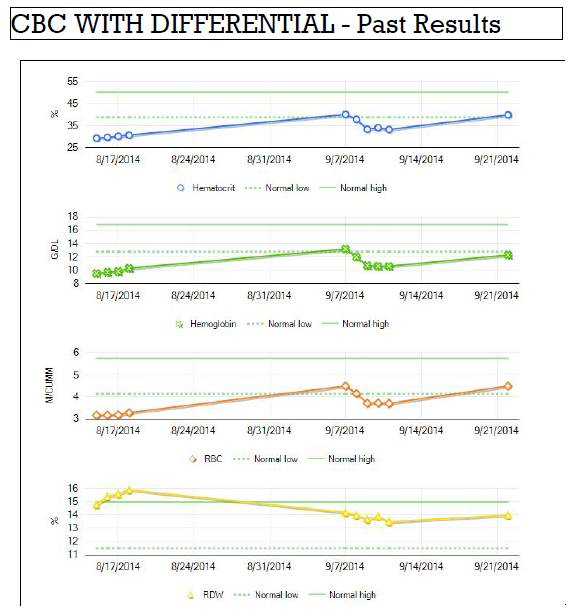
The charts below show how my blood responded after my surgery on 8/11. Of course during surgery I lost blood. It looks like my hemoglobin dropped close to 9 g/dL (grams per deciliter). Since the normal range for men on this test is 14-17, I was anemic.
Between my release from the hospital on Monday 8/18 and my hospital admission on Sunday 9/7 my hemoglobin, hematicrit, and other numbers for oxygenation all returned to the low end of normal. However, during my hospital stay in September, my hemoglobin and other numbers dropped again.
I've gotten these definitions from WebMD.
Hematocrit
Hematocrit is a measure the volume taken by the red blood cells. The Hematocrit is a measure which combines the information from the RBC and MCV measures. Low Hematocrit indicates anemia.
Hemoglobin
Hemoglobin is the protein that carries oxygen in the blood. Low hemoglobin indicates anemia.
RBC
Red blood cell count measures the number of red blood cells in the sample blood. Low RBC indicates anemia.
RDW
The Red blood cell distribution width gives a measure of the disparity in red blood cell sizes. If you have lots of large and small red blood cells, this number would be large. If your red blood cells are all around the same size, then the number will be small. High RDW, may indicate you have been bleeding
MCH
Mean corpuscular hemaglobin indicates the hemaglobin in the average red blood cell. In my charts above this value is dropping - which makes sense to me if I hadn't been taking iron (my body would be creating red blood cells but I wouldn't have enough iron to create the hemaglobin for them).
MCHC
Mean corpuscular hemaglobin concentration indicates the concentration of hemoglobin in the average red blood cell.
MCV
Mean corpuscular volume indicates the size of the red blood cells. Smaller size indicates younger cells which may mean the patient is having to replace lost blood.
Because of this persistent anemia, I've begun treating myself (with my doctor's permission) by taking iron supplements. I understand why my hematocrit and hemoglobin are responding in the manner shown in the charts but I do not understand why my MCH and MCHC continue to decline despite taking iron supplements.
Anemia may be subdivided into the following levels
Mild anemia: hemoglobin 10 to 11 g/dL
Moderate anemia: hemoglobin 8 to 10 g/dL
Severe anemia: hemoglobin 6.5 to 8 g/dL
Life-threatening anemia: hemoglobin less than 6.5
From doing research on the topic and also experimenting upon myself when I've been anemic in the past, I've found that taking these vitamin supplements aids in both the absorption of iron and reduces the adverse side-effects of the iron supplements (cramping, constipation, and other related issues):
Vitamin C
Vitamin B12
Folic Acid
I've been advised to not take more than 800 mcg of Folic Acid in a week.
Between my release from the hospital on Monday 8/18 and my hospital admission on Sunday 9/7 my hemoglobin, hematicrit, and other numbers for oxygenation all returned to the low end of normal. However, during my hospital stay in September, my hemoglobin and other numbers dropped again.
Hematocrit
Hematocrit is a measure the volume taken by the red blood cells. The Hematocrit is a measure which combines the information from the RBC and MCV measures. Low Hematocrit indicates anemia.
Hemoglobin
Hemoglobin is the protein that carries oxygen in the blood. Low hemoglobin indicates anemia.
RBC
Red blood cell count measures the number of red blood cells in the sample blood. Low RBC indicates anemia.
RDW
The Red blood cell distribution width gives a measure of the disparity in red blood cell sizes. If you have lots of large and small red blood cells, this number would be large. If your red blood cells are all around the same size, then the number will be small. High RDW, may indicate you have been bleeding
MCH
Mean corpuscular hemaglobin indicates the hemaglobin in the average red blood cell. In my charts above this value is dropping - which makes sense to me if I hadn't been taking iron (my body would be creating red blood cells but I wouldn't have enough iron to create the hemaglobin for them).
MCHC
Mean corpuscular hemaglobin concentration indicates the concentration of hemoglobin in the average red blood cell.
MCV
Mean corpuscular volume indicates the size of the red blood cells. Smaller size indicates younger cells which may mean the patient is having to replace lost blood.
Because of this persistent anemia, I've begun treating myself (with my doctor's permission) by taking iron supplements. I understand why my hematocrit and hemoglobin are responding in the manner shown in the charts but I do not understand why my MCH and MCHC continue to decline despite taking iron supplements.
Anemia may be subdivided into the following levels
Mild anemia: hemoglobin 10 to 11 g/dL
Moderate anemia: hemoglobin 8 to 10 g/dL
Severe anemia: hemoglobin 6.5 to 8 g/dL
Life-threatening anemia: hemoglobin less than 6.5
From doing research on the topic and also experimenting upon myself when I've been anemic in the past, I've found that taking these vitamin supplements aids in both the absorption of iron and reduces the adverse side-effects of the iron supplements (cramping, constipation, and other related issues):
Vitamin C
Vitamin B12
Folic Acid
I've been advised to not take more than 800 mcg of Folic Acid in a week.

No comments:
Post a Comment